Introduction: HbSC is a common form of sickle cell disease especially prevalent in West Africa. Despite experiencing similar clinical events as those with sickle cell anemia (HbSS or HbSβ 0 thalassemia), individuals with HbSC disease have received much less attention because disease complications occur less frequently and often manifest later in life. Retrospective reports suggest that hydroxyurea might benefit people living with HbSC disease, but rigorous prospective data are unavailable to describe potential treatment benefits, long-term safety, and appropriate study endpoints. We designed a Phase II clinical trial of hydroxyurea for children and adults with HbSC disease with the following aims: 1) to measure possible laboratory toxicities of hydroxyurea; 2) to assess the clinical effects of hydroxyurea on sickle-related clinical and laboratory parameters; and 3) to identify study endpoints that are suitable for a future definitive Phase III trial of hydroxyurea for HbSC disease.
Methods: Prospective Identification of Variables as Outcomes for Treatment (PIVOT, Trial ID PACTR202108893981080) is a double-blind, randomized, placebo-controlled Phase II trial of hydroxyurea. Inclusion criteria included people with HbSC disease, age 5 to 50 years, receiving care at Korle Bu Teaching Hospital, Accra, Ghana. Exclusion criteria included treatment with hydroxyurea or other disease-modifying treatment or participation in a therapeutic trial in the previous 6 months, hospitalization >10 times in the past 12 months, pregnancy, severe chronic kidney disease or other underlying illness making participation ill-advised, previous myelosuppressive therapy or stem cell transplant, or inability to take hydroxyurea. After written informed consent, participants underwent initial screening for 2 months before randomization to placebo or hydroxyurea (donated by Addmedica, Inc, Paris) with a goal of treating ~100 participants in each arm for one year. Randomization is stratified by age and sex to ensure equal numbers of children and adults with balanced baseline characteristics in each arm. The primary study outcome is cumulative hematological toxicities after 12 months of treatment. Here we report the baseline characteristics of the enrolled cohort.
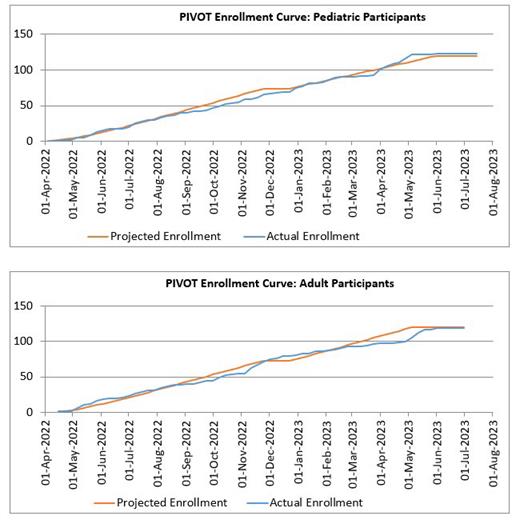
Results: From April 2022 to June 2023, a total of 243 patients with HbSC disease (123 children, 120 adults) consented and began screening (Figure); after ~10% screen failures, 217 (112 children, 105 adults) were eligible for randomization. The average age (mean ± SD) at enrollment was 21.9 ± 14.6 years and 47% were female. Baseline medical history documented that almost all study participants (93%) reported previous hospitalization, while 87% had previous vaso-occlusive events, 78% had malaria, 21% reported transfusion, and 1 patient had a stroke. Baseline labs included hemoglobin = 11.0 ± 1.3 g/dL, HbF = 1.8 ± 1.5 %, ANC = 3.7 ± 1.8 x 10 9/L, and platelets 269 ± 115 x 10 9/L. Additional baseline laboratory studies include whole blood viscosity, ektacytometry, and point-of-sickling. Baseline assessment revealed a palpable spleen in 6 children (5%) and 1 adult (1%), but abdominal ultrasonography documented splenic tissue in 97% of children and 83% of adults with an average volume of 116 ± 71 mL (range 13 - 354 mL) and 222 ± 165 mL (range 4 - 707 mL), respectively. TCD examinations on children revealed an average maximum time-averaged mean velocity of 111 ± 19 cm/sec with 98% normal exams, 1% conditional, 0% abnormal, and 1% inadequate. Retinopathy was identified in 46% of children and 85% of adults, including both proliferative and non-proliferative findings. Near Infrared Spectrometry (NIRS), 6-minute walk, and Quality of Life were also collected.
Discussion: Individuals with HbSC endure a substantial number of life-altering clinical complications and early mortality. Better treatments for this large group of people are desperately needed, and hydroxyurea is an obvious choice due to its low cost and ease of oral administration. Better understanding of the rate and severity of disease manifestations across the age span is needed to more completely understand the best time to treat this group to mitigate complications. Now fully enrolled, PIVOT will provide invaluable insights into the effects and potential benefits of hydroxyurea on clinical and laboratory outcomes among people living with HbSC disease.
OffLabel Disclosure:
Amissah-Arthur:Optos, Inc: Research Funding. Latham:Emmaus Medical: Research Funding. Ware:Emmaus Medical: Research Funding; Addmedica: Research Funding.
Hydroxyurea is approved for HbSS disease. This trial will investigate its use for HbSC disease.